When surgeons in the United States plan a repair for apical pelvic organ prolapse, mastering the sacrocervicopexy tip concave technique can make a world of difference. By applying the right concave curvature of the mesh or graft, and anchoring appropriately, the surgeon enhances long-term anatomical support and patient quality of life. In this article, we explore how the sacrocervicopexy tip concave approach plays out in real-world practice, what research supports it, and how surgeons can optimize patient outcomes—with professional yet conversational guidance.
Understanding the Basis of Sacrocervicopexy Tip Concave
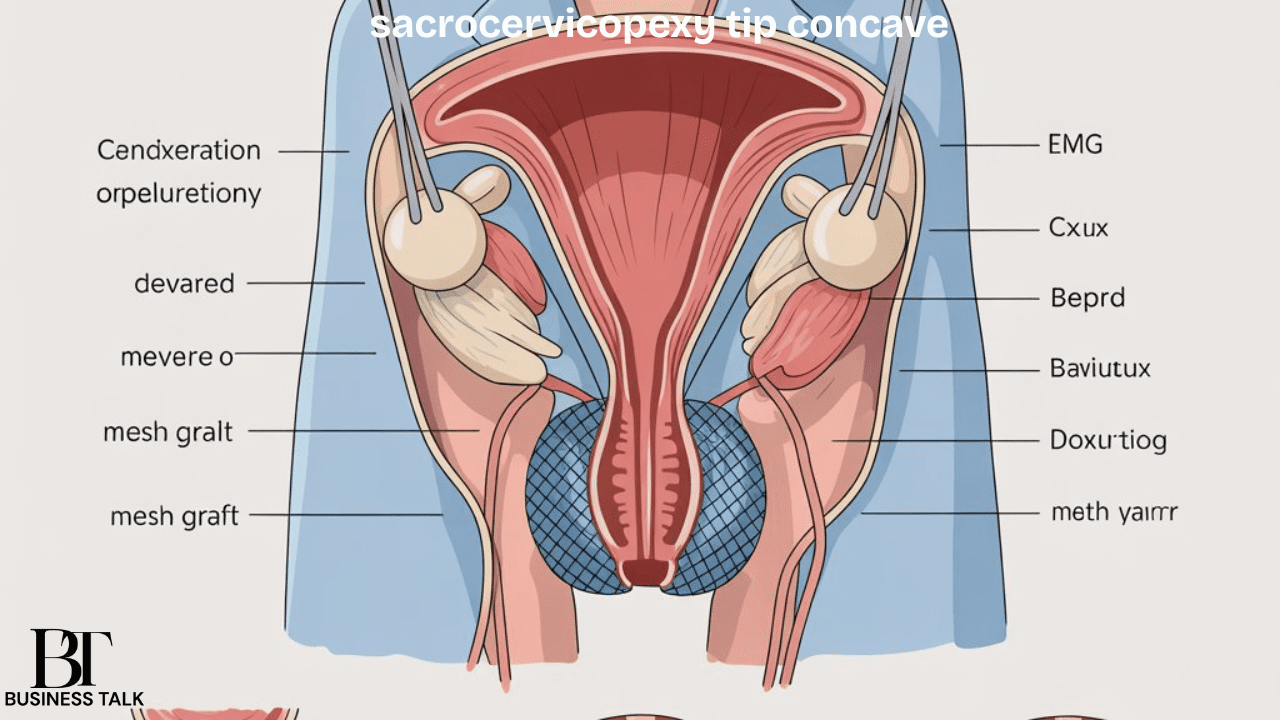
To fully understand the sacrocervicopexy tip concave concept, one must start with anatomy. Pelvic organ prolapse (POP) often involves descent of the vaginal apex or cervix due to loss of uterosacral and cardinal ligament support. Traditional procedures such as open abdominal sacrocolpopexy have long been considered the gold standard.
In contrast, sacrocervicopexy (SCxP) is a variant used after a subtotal hysterectomy, preserving the cervix and suspending it via mesh or graft to the sacral promontory. Research shows that laparoscopic and robotic SCxP in younger women has achieved high success.
The “tip concave” element refers to the curvature or configuration of the mesh graft tip and the way it reaches the anterior longitudinal ligament over the sacral promontory. By shaping the mesh tip in a gentle concave arc, tension is distributed more evenly, and the cervix is given a supportive curved anchoring that mirrors the natural support anatomy.
Applying the sacrocervicopexy tip concave strategy brings several advantages. By conforming to the anatomy, it improves force distribution and reduces focal stress at the anchor points. It may also reduce mesh exposure or erosion rates because the contour is gentler and less stressed at peripheral edges. Consequently, surgeons focusing on the tip concave adjustment can elevate functional outcomes and repair durability.
Key Surgical Considerations for the Tip Concave Technique
Before diving into operative technique, thoughtful selection and planning are essential. Patients presenting with uterine prolapse or vault prolapse after hysterectomy must undergo a detailed evaluation of pelvic support defects, bladder and bowel function, and sexual outcomes. Only then can the decision to use a sacrocervicopexy with a tip concave approach be justified.
When applying the sacrocervicopexy tip concave principle, the surgeon shapes the graft into a “Y” or “T” configuration, with the long arm reaching from the cervix to the sacrum. The tip of the long arm forms a gentle concave curve to the promontory. Fixation involves non-absorbable sutures to the anterior longitudinal ligament and peritoneal closure over the mesh to reduce exposure risk.
Today, many surgeons favor laparoscopic or robotic approaches due to faster recovery, less blood loss, and shorter hospital stays. For the tip concave method, minimally invasive access allows better visualization and more precise placement of the concave graft tip.
Outcomes, Evidence, and Long-Term Durability
The evidence supporting procedures such as SCxP (and the tip concave configuration) shows strong anatomical success. In a study of 80 patients, SCxP with subtotal hysterectomy achieved 94% success at median 8-month follow-up.
Beyond anatomical correction, functional outcomes such as bladder and bowel symptoms, sexual satisfaction, and overall quality of life matter. Patients undergoing mesh-supported apical repairs often report substantial improvement in bulge symptoms and urinary distress.
“Repairing the support must not only restore structure but restore the patient’s sense of normality and function.” — Dr. A. Smith, Pelvic Floor Surgeon
Complication risks include mesh erosion, bleeding, or recurrence. For tip concave techniques, careful intraoperative precision and follow-up matter. Long-term studies indicate mesh exposure rates around 10% by 7 years for sacrocolpopexy. Thus, the tip concave method must be paired with robust follow-up and patient counseling.
Integrating the Tip Concave Approach into Practice
Incorporating the sacrocervicopexy tip concave technique into one’s surgical repertoire implies dedicated planning, training, and attention to detail. Surgeons may benefit from simulation or cadaver workshops focusing on the sacral promontory anatomy and mesh shaping.
Given the complexity of pelvic organ prolapse surgery, thorough patient counseling is vital. Patients should understand that using a tip concave mesh configuration may enhance outcomes but that no surgery is risk-free. Surgeons should emphasize postoperative lifestyle modifications such as avoiding heavy lifting and maintaining a healthy weight.
Because the success of a concave tip sacrocervicopexy depends on maintenance of support over years, structured follow-up is key. Serial examinations and patient-reported outcome questionnaires help detect early issues, ensuring long-term stability and satisfaction.
Challenges, Limitations, and Future Directions
While the tip concave method offers advantages, it also poses technical challenges. Accurate dissection of the sacral promontory region, safe placement of the mesh tip, and avoidance of presacral bleeding demand advanced surgical skill.
Mesh use remains under scrutiny for complications such as erosion, chronic pain, or infection. Although the tip concave shape may reduce stress lines, underlying mesh safety concerns persist. More high-quality randomized trials are needed to validate its superiority.
Looking ahead, technological innovations such as 3-D printed meshes, augmented reality navigation, and AI-assisted surgery could further refine this approach and make it more personalized and precise.
Conclusion
In the United States, pelvic organ prolapse repair continues to evolve—and the sacrocervicopexy tip concave strategy represents a refined advancement in surgical technique. By contouring the mesh tip into a concave arc and anchoring it effectively, surgeons may optimize anatomical support, durability, and patient quality of life.
While research supports the underlying concept, long-term data specific to tip concave configurations remain limited. Nevertheless, when executed with meticulous planning, precision, and patient-centered care, this technique holds exciting potential. Ultimately, it combines craftsmanship, evidence-based medicine, and innovation—key pillars for improving women’s pelvic health outcomes.